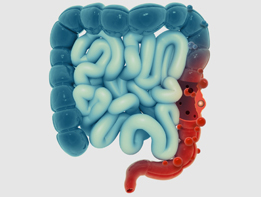
Diverticulitis of Colon
Colonic diverticulitis is a condition commonly affecting individuals consuming a low fiber diet. Low dietary fiber can result in constipation and increased pressure within the lumen of the colon. This can cause protrusion of the inner layer of the colon through weak areas within the wall of the colon, as small outpouchings called diverticula. When multiple diverticula are present, the condition is called diverticulosis. When the diverticula become inflamed or infected, the condition is called diverticulitis. Diverticular disease is a term that includes both diverticulosis and diverticulitis.
Many patients have diverticular disease without symptoms. Other patients may experience signs and symptoms of diverticulitis as a result of inflammation and infection of the diverticula and the surrounding segment of colon. These include abdominal pain, fever, nausea, vomiting, change in bowel habits, bloating, etc. Patients with diverticulosis may experience bleeding. Bleeding is usually in the form of bright red blood per rectum and may be brisk.
Most patients with diverticular disease do not experience complications related to the disease. However, those who do are subject to potentially serious complications. These include:
- Infection: The most common form of infection is segmental inflammation and infection without perforation. This is called non-complicated diverticulitis. It is treated by bowel rest and a course of antibiotics. The usual duration of an acute episode of diverticulitis is 1-2 weeks. Sometimes, severe infection may result in perforation of a diverticulum. This is called perforated diverticulitis. Majority of perforations are microscopic and spontaneously walled off by body’s own surrounding tissues. The resultant phlegmon (indistinct mass) is treatable by antibiotics. If the size of perforation is large, it will result in an abscess (collection of infected fluid). An abscess requires drainage by an interventional radiologist via a percutaneous approach, and antibiotic treatment. The most severe type of perforation is when there is free spillage of stool within the peritoneal cavity, resulting in peritonitis and sepsis. This requires emergency surgery and often a colostomy.
- Bleeding: Colonic diverticula are closely associated with blood vessels of the colon. Inflammation of diverticula may result in bleeding. Diverticular bleeding is often brisk and severe, requiring hospitalization and blood transfusion. Sometimes, if the bleeding does not respond to non-surgical treatment, emergency surgery may be required.
- Obstruction of colon: As a result of repeated attacks of diverticulitis, colonic lumen may get narrowed to a point where stool may no longer pass easily, resulting in obstruction. This presents as inability to completely evacuate with bowel movements. Colonic obstruction is an indication for surgery.
- Fistula: Sometimes, an inflamed segment of colon gets attached to a neighboring structure. Over time, an abnormal communication may form between the two structures. This is called a fistula. The most common type of fistula is a colo-vesical fistula, formed between the colon and the urinary bladder. Patients present with pneumaturia (passage of gas while urinating) and urinary tract infection. This is an indication for urgent surgery.
Diverticular disease is often diagnosed clinically. It can also be identified during a colonoscopy or a CT scan. If the disease is identified during a routine colonoscopy and patient has not history to suggest prior symptoms, no further treatment is required except increasing dietary fiber and avoiding nuts and seeds.
However, if a patient has had at least several episodes of acute diverticulitis, surgery may be indicated electively to prevent future attacks or to prevent complications. If a patient presents with any of the complications listed above, surgery may be required emergently.
Minimally invasive colectomy is the procedure in which the affected segment of colon is removed surgically using very small incisions and minimally invasive techniques. It can be performed with either laparoscopic or robotic approach. These two approaches are very similar, as they both reduce post-operative pain and shorten the recovery process, when compared with open colectomy. Robotic colectomy, as compared to laparoscopic colectomy however, has the added advantage of providing instruments with wristed motion for complex maneuverability, and 3D optics with 10X magnification for precise visualization and depth perception. Robotic stapling platform identifies tissue thickness and aids in preventing misfires. As a whole, robotic approach increases precision, decreases potential trauma, and enhances the recovery process.
Dr. Zaré has been performing minimally invasive colon resection since 2002, accumulating a large experience with various laparoscopic approaches including hybrid, hand-assisted, and intra-corporeal approaches. In 2014, thanks to advances in robotic technology, he began offering robotic colon resections, performing some of the earliest robotic colectomies in Northern California. While patients undergoing laparoscopic colon resection already experience superior outcomes compared to their open counterparts, those undergoing robotic surgery experience even better outcomes. For example, the average length of stay for open colon resection is 7 days. It is reduced to 4 days for laparoscopic resection, and 2-3 days for robotic resection. The need to convert to open surgery occurs in less than 5% of the procedures.
If the procedure is performed electively when the colon is not inflamed or infected, your surgeon can remove the diseased segment of the bowel and reattach the unaffected parts together, all in one stage. It is therefore important to seek surgical advice if you meet any of the indications listed above, and before the onset of the next attack.
If surgery has to be performed during an active bout of inflammation or when the overall hemodynamic condition of the patient is unfavorable as a result of systemic infection, a temporary colostomy is usually created. A colostomy is created when the top portion of the colon is brought out through a hole in the abdominal wall into a bag. Patient will then require a second operation after two to three months to reattach the healthy segments. This is called a two-stage approach, which can be avoided in many instances.