Laparoscopic Groin or Inguinal Hernia Repair
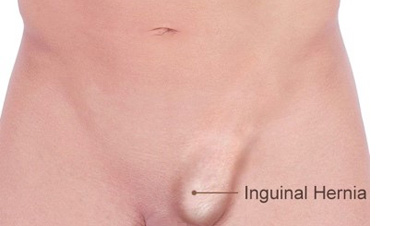
Groin or Inguinal hernia is the most common type of hernia. It occurs when contents of the abdomen protrude as a bulge through a weakness in the muscles of the groin. Some individuals are born with hernias at birth and exhibit signs and symptoms during childhood or later in life. Others acquire hernias during adulthood as a result of wear and tear of abdominal wall musculature, especially if they have active lifestyles. Inguinal hernia may occur in one or both groins, initially starting as a small painless bulge, and over time growing in size and becoming symptomatic. Sometimes it may be associated with serious complications like bowel obstruction or strangulation.
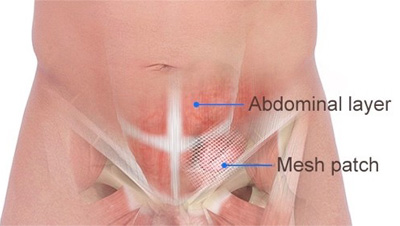
Fortunately, inguinal hernia can be repaired laparoscopically. Because laparoscopic repair is a tension-free repair performed through very small incisions, it is not associated with much post-operative pain. The procedure is performed at an ambulatory surgery center and the patient is discharged home within an hour of surgery. Patients may resume day-to-day activities after one day and unlimited activities after one week. In experienced hands, laparoscopic inguinal hernia repair is extremely safe and has a very low rate of recurrence. Based on the nature, location, and size of your hernia, Dr. Zaré will recommend either a laparoscopic or open repair. Majority of patients are candidates for laparoscopic repair. In rare instances, due to prior open procedures in the lower abdomen such as radical prostatectomy, hysterectomy or colon resection, the resultant scar tissue prohibits a laparoscopic approach. In these instances, an open approach will be used.
Dr. Zaré has been performing the gold standard approach for laparoscopic inguinal hernia repair called Laparoscopic totally extra-peritoneal (TEP) approach since 2002. In the TEP approach, the surgeon makes 3 small incisions in the midline below the umbilicus and gains access to the groin via the layers of abdominal wall and without invading the peritoneal cavity, hence the term ‘totally extra-peritoneal’. Using this approach, repair of hernia can be performed with the absolute minimum interruption of anatomic structures. With the alternative approach called Laparoscopic trans-abdominal pre-peritoneal (TAPP) approach, surgeon makes the same number of incisions, but enters into the peritoneal cavity, potentially handles bowel and intra-abdominal adhesions, then divides the peritoneal layer, gains access to the groin, and at the termination of the procedure sews the peritoneal layer back in place. These additional steps increase the potential for post-operative complications and pain. Since the early 1990’s, the two laparoscopic approaches have been studied extensively, and the laparoscopic TEP repair has been found to be associated with superior outcomes.
Due to the technical nature of laparoscopic TEP repair, surgeons are required to perform 250-500 cases in order to gain proficiency in this technique. Dr. Zaré has successfully performed over 3,000 TEP repairs and has one of the largest experiences of laparoscopic inguinal hernia repair in San Jose and the San Francisco Bay area. His outcomes compare favorably with nationally reported data.
Recently, robotic surgery for hernia repair has gained popularity, especially among surgeons performing open hernia repair. Although Dr. Zaré is an early adopter of modern robotic surgery in the South Bay area - having performed the first robotic colon resection and repair of hiatal hernia with fundoplication at Good Samaritan Hospital - he does not offer robotic inguinal hernia repair. After a careful study of the role of robotic surgery in this specific area, we concluded that laparoscopic inguinal hernia repair is superior to robotic inguinal hernia repair in our practice. The reason is that while laparoscopic inguinal hernia repair is preferentially performed via the gold standard TEP approach, robotic inguinal hernia repair is usually performed via the TAPP approach, which is more invasive and is associated with inferior outcomes (see above).